Are Statins the Answer?

Statin drugs are one of the most prescribed medicines in the United States. Statins are two of the top 10 prescribed medications in the United States (Lipitor and Zocor). Lipitor is the #1 prescribed medication in history, with total sales of $150 billion. This cost is staggering.
Statins have been available for use by prescription since September 1, 1987. For the last 35 years, they have been prescribed by physicians under the pretense that they protect patients from heart attacks and progressive coronary artery disease.
I began practicing cardiology in 1983. When statins first became available, it was a common assumption by cardiologists that statin drugs could eliminate or dramatically lower the incidence of acute and chronic coronary artery disease. This belief was based on the premise that most heart disease was related to cholesterol abnormalities. It was a surprising conjecture because there was clear evidence that underlying inflammation was the primary cause of this common disease.
Over the last three decades, my perspective and statin utilization have changed dramatically. Initially, I was willing to do anything to help my patients alleviate their risk and diminish the frequency of heart attacks. As an interventional cardiologist who spent many hours in the cardiac catheterization laboratory treating patients with severe coronary artery disease and acute heart attacks, any medical treatment that would alleviate this disease was a welcome balm. We were surrounded and inundated with the positive benefits of statin therapy by pharmaceutical representatives and articles in our medical literature. Statins could do no wrong. The benefits were overwhelming, and the side effects were minimal.
Interestingly, my initial experience with statin side effects seemed contrary to the reported low incidence of muscle aches, cognitive issues, and fatigue. My patients seemed more willing to discontinue the medication than to accept the risk
reductionbenefits. Like many physicians, I was too busy to scrutinize the medical literature regarding this phenomenon and wanted to do everything to help my patients.
Several years ago, I came across a critical analysis of the Jupiter trial. In that trial, the subsequent analysis over the years revealed that Crestor (a newer statin) did not have the benefits widely reported during the initial reports. I was astonished that such deception had occurred, making me look much more critically and analytically at the medical literature. It provoked me to analyze the risks and benefits of statin therapy more carefully.
I have significantly altered my approach to statin therapy after intensive education. This decision has come after much thought, clinical experience, and review of an extensive body of literature. Many of my fellow cardiologists would be surprised at my cynicism toward statin therapy, and I cannot blame them for this view. There is a long-held belief by the cardiology community that statins are the golden egg provided for the successful treatment of heart disease. Interestingly, however, the incidence of cardiovascular disease has remained relatively high since 1987, and this realization seems to go unnoticed by my colleagues. Despite this finding, beliefs and habits are tough to alter. Mark Twain observed,
“The glory which is built upon a lie soon becomes a most unpleasant incumbrance. … How easy it is to make people believe a lie, and how hard it is to undo that work again!”
Over the last several years, one of my patients’ most common questions is whether they should start or continue prescribed statin therapy. There is a significant amount of concern by the non-medical community regarding statins, including their potential risks and benefits. Patient confidence in statin therapy in the United States is reportedly low. Patient compliance with taking statins is approximately 50%. Patients may hesitate to take the medicines or experience unspoken side effects. Cost may also be an issue in some cases. Based on my clinical experience, I suspect the side effect profile is more significant than reported in the medical literature. In addition, I believe the patients have significant concerns regarding the risks and benefits of these drugs. Sadly, some physicians advise patients to maintain statin therapy even in the presence of ongoing intolerance. In addition, many excellent physicians feel pressured to “meet the guidelines,” and statin utilization is part of the guideline requirement for patients with elevated cholesterol and diabetes.
I want to provide some perspectives on statins I have developed over my clinical career. To some, these observations may be based on misconceptions and misunderstandings of the literature. I will leave that up to the reader, but a lifetime of experience with these agents has failed to convince me of the suggested lifesaving benefits. I have spent an extended time investigating both sides of this issue. I believe it is imperative to seek the truth to avoid biases and preconceptions that may cloud one’s perspective. As a physician, I am very blessed to be asked for my advice. I would never want to mislead a patient falsely for any reason. Shared decision-making is a critical factor underutilized by the medical profession.
So here goes:
The most current diseases that we face as physicians are metabolic diseases, which include diabetes, cardiovascular disease, hypertension, obesity, and thyroid disease. More than 90% of the US population is estimated to suffer from suboptimal cardiometabolic health. This number is staggering.
Inflammation and insulin resistance are the underlying cause of almost all of the above diseases. In addition, poor nutrition, a sedentary lifestyle, chronic stress, and poor sleep habits are linked to inflammation and contribute to poor cardio-metabolic status.
At a cellular level, mitochondrial dysfunction appears to be the primary consequence that results in metabolic abnormalities. The mitochondria are the engines in each cell, and mitochondrial function is vital to cellular and overall metabolic health. Mitochondrial dysfunction occurs in all of the above disease states. Significantly, lifestyle changes and specific supplements can reverse underlying mitochondrial dysfunction.
Statins directly affect mitochondrial function and appear to cause dysfunction in various ways. Although the following diagram from the Journal of Cachexia, Sarcopenia, and Muscle may seem confusing, it reveals how statins affect mitochondrial function.
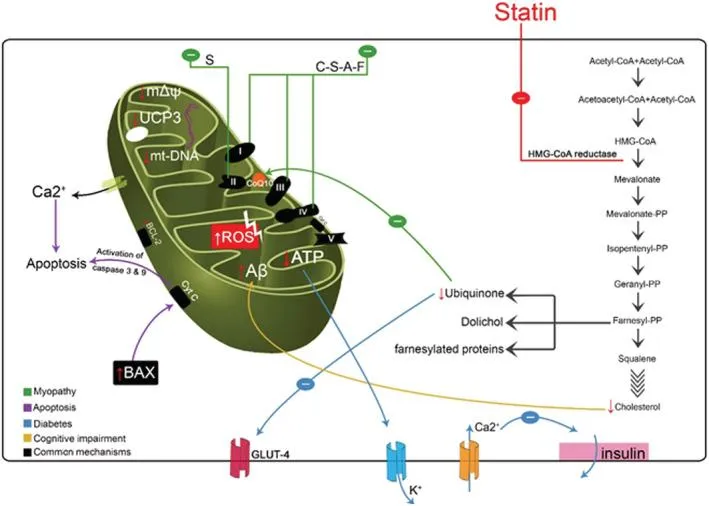
Effects of statins on mitochondrial function: (i) reduction in mitochondrial membrane potential; (ii) reduction in coenzyme Q10 (CoQ10) and GLUT‐4 expression; (iii) increased reactive oxygen species (ROS) level and induction of intrinsic apoptosis; (iv) deregulation of Ca2+ metabolism; (v) mitochondrial depletion; (vi) decrease in uncoupling protein 3 (UCP3) expression and reduction in β‐oxidation efficiency; (vii) increase in amyloid‐β (Aβ) concentration in mitochondria; (viii) direct inhibition in respiratory chain. A, atorvastatin; C, cerivastatin; F, fluvastatin; HMG‐CoA, β‐hydroxy β‐methylglutaryl‐coenzyme A; mtDNA, mitochondrial DNA; PP, pyrophosphate; S, simvastatin.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8061391/
Statins cause muscle-related abnormalities that are probably linked to coenzyme Q 10. Supplementation with this enzyme alters some of the muscular side effects of the drugs. The diagram reveals how coenzyme Q 10 is effectively blocked from production by statin therapy.
Statins are also linked to insulin resistance, diabetes provocation, and obesity. As can be seen from the diagram, these effects are primarily related to a cellular influence. There has been a rather dramatic increase in the incidence of diabetes over the past two decades. This increased risk is undoubtedly associated with higher sugar intake and dietary changes that enhance the risk of insulin resistance. People with diabetes are targeted for the institution of statin therapy, even in the absence of documented CAD. The paradox here is that diabetes can be provoked in some patients on statin therapy. Why would you start a drug that can potentially cause or aggravate another metabolic disease? Pharmaceutical companies and “experts” try to minimize this risk, but the evidence appears clear.
LDL-cholesterol does have some pro-inflammatory features, but LVL also appears to play a role in enhancing immunity in elderly patients. There is a link between the risk of infection in older individuals and statin therapy, especially bacterial infections. One well-controlled study in 2021 examined the risk of death in statin users hospitalized with COVID-19. The average patient age was 70 years. There was a significant increase in mortality at 28 days in this patient population. The minimal benefit of statin therapy in older patients based on mortality studies would suggest that statins should be avoided unless there is clear evidence of ongoing symptomatic cardiovascular illness.
Statin therapy has been implicated in cognitive abnormalities. My experience suggests that it is somewhat less common than patients may assume, but there is reasonable evidence to suggest cognitive dysfunction can occur in some patients. The provocation of cerebral abnormalities in older patients may lead to extensive testing to exclude dementia and instill fear and concern in patients and families. Additionally, physicians may be hesitant to discontinue these medications under the pretense that Alzheimer’s patients benefit from statins. Alzheimer’s is a nonvascular cause of dementia, and statins are ineffective. Stopping statin therapy is one of the first things I do in patients complaining of cognitive or mood-related issues.
Falls are a significant cause of injury in the elderly. The risk of falling is related to many factors, including loss of muscle tone and strength and progressive gait instability. A hip fracture resulting from falls in the elderly is associated with a 5 to 8-fold enhanced risk of death in the first three months after the injury, especially among men. Statin therapy has been shown to impair balance in the side-to-side direction in some patients. This effect can lead to an enhanced fall and fracture risk, including falls on the hip and leg. Avoiding any drug therapy that significantly increases fracture risk and mortality seems intuitive. This is another reason to consider discontinuing statin therapy in my older patients when the risk-benefit ratio seems “unbalanced.”
It is crucial to know if statin therapy will prolong life and at what cost regarding compliance and side effects. What may surprise many patients is that the average number of days that statin therapy may prolong life in those without documented coronary artery disease is approximately four days. In patients who have taken statin therapy for 20 years, this averages about two weeks of extended life. Would patients agree to take statins and tolerate the associated side effects for 20 years if they knew the actual impact on longevity?
The number needed to treat (NNT) is a statistical measurement utilized to compare the effectiveness of a drug or intervention. I have found it to be a valuable tool when assessing statin drugs’ efficacy. A website (TheNNT.com) compares various clinical situations and the NNT related to those conditions. In addressing the value of statin therapy for preventing cardiac events in patients without documented heart disease, utilized this measurement, and others concluded that no lives were saved when patients used statins for five years in this group. One in 60 patients suffered a nonfatal heart attack, while one in 268 was rescued from a stroke. Notably, one in 67 was harmed by diabetes, and one in 10 developed muscle damage while on the drug for five years. It is clear from these numbers that it is more likely that statin therapy will provoke diabetes compared to preventing a nonfatal heart attack. In addition, statins will not save lives based on this analysis. Isn’t that the most important statistic of all?
The numbers are not much better in patients with established coronary artery disease. This group included only those patients with a previous heart attack. 96% of patients who took statins five years experienced no benefit, while 1.2% avoided death and 2.6% benefited from avoidance of a second heart attack. 0.6% of this group develop diabetes. It must be stated, however, that the benefits in this group are comparable to the results in patients who engaged in cardiac rehabilitation following their heart attack. Importantly, cardiac rehabilitation did not provoke or worsen diabetes. This benefit makes sense because exercise is one of the most significant ways to avoid insulin resistance and future diabetes.
It is known that statins increase coronary artery calcification. This appears to be related to the effect of statins on vitamin K2 availability. Vitamin K2 activates a protein called GLA protein matrix that reduces the risk of arterial calcification. High-dose statins have a particular propensity to enhance coronary artery calcification. Scientists feel that this adverse effect is offset by the statin-induced reduction in soft cholesterol plaque within the artery. It is known that cardiac events such as heart attacks, bypass surgery, and the need for coronary stents are increased in patients with high calcium scores. This coronary-calcium paradox is well described, but most researchers and cardiologists need more clarification about the long-term detrimental effects of increased calcium within the coronary arteries. I do not believe in medical “paradoxes,” I feel these are simply excuses for things that don’t make sense or cannot be explained. I am not an engineer, but also concerned about enhancing someone’s coronary artery calcium with statins. The laws of hydrodynamics suggest that pulsatile flow in a distensible tube (coronary artery) will be adversely affected if that artery becomes more rigid from excess calcification. This may lead to undesirable flow turbulence and coronary artery perfusion abnormalities. That seems like a bad idea.
Dementia seems to be in many people’s minds as they grow older. There have been questions about the role of statin therapy in patients with dementia. Alzheimer’s dementia is the most common type of dementia and does not appear to have a vascular basis. Consequently, statin therapy would not seem to have any benefit and does not appear to have any role in treatment or prevention. More interesting, however, is that patients with familial hypercholesterolemia (those with very high cholesterol) do not appear to be at higher risk for dementia. Vascular dementia is much less common but has a basis related to narrowing the arteries within the brain. How can patients with the highest cholesterol levels possibly avoid vascular dementia? This exciting fact again raises the question of whether cholesterol truly is the primary cause of underlying atherosclerosis or narrowing of the arteries. Statins appear to have no valid role in dementia treatment. I generally avoid this therapy in my patients with cognitive decline unless they have solid evidence of severe and symptomatic cardiovascular disease.
I have evolved from a strong advocate to a questioning agnostic. There are certainly some limited benefits from this group of drugs. Still, most patients with and without cardiovascular disease have many other options to reduce their risk. Most of these options do not include any pharmaceutical agents and are focused on lifestyle modification. The principal role of a physician is to provide healing. Healing involves identifying and treating factors causing the underlying medical condition. Cardiovascular illness is often successfully treated with changes in diet, activity levels, sleep enhancement, and stress reduction. As I continue to evolve in my knowledge of cardiovascular disease, it has become abundantly clear that fewer drugs and more good lifestyle habits are the key to long-term treatment and healing. The long-term benefits can be remarkable for patients willing to make some lifestyle adjustments. For those who have no desire to change their bad habits, statin therapy may offer minimal benefit but at some risk. As always, the individual patient will be the impetus for the treatment. The principles of shared decision-making should always guide the essence of the decision to treat or not to treat. The foundation for these decisions must be grounded in full knowledge of the risks and benefits of any long-term treatment option. As physicians and healers, we must share this information objectively and clearly. Only then can patients and physicians walk together in seeking optimum health and happiness.
Empower yourself with holistic, lifelong health.
Click below and change your life for good
More than 200,000 people agree
that we are different
“Lorem ipsum dolor sit amet consectetuer adipiscing elit. Aenean commodo ligula eget dolor.“
GYMNASTICS COACH
Sarah North
Testimonial

John Doe
Finance Manager
Lorem ipsum dolor sit amet, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa. Cum sociis natoque penatibus et magnis dis parturient montes, nascetur ridiculus mus.

John Doe
Finance Manager
Lorem ipsum dolor sit amet, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa. Cum sociis natoque penatibus et magnis dis parturient montes, nascetur ridiculus mus.

John Doe
Finance Manager
Lorem ipsum dolor sit amet, consectetuer adipiscing elit. Aenean commodo ligula eget dolor. Aenean massa. Cum sociis natoque penatibus et magnis dis parturient montes, nascetur ridiculus mus.

